Aetna Claim Denial Codes 64 - Remittance advice (ra) remark codes are two to five characters and begin with n, m, or ma. This is the complete list of denial codes (claim adjustment reason codes) with an explanation of each denial. Jan 1, 1995 · these codes describe why a claim or service line was paid differently than it was billed. If there is no adjustment to a claim/line, then there is no adjustment reason code. Remark code m64 indicates that the claim has been processed with an issue related to the other diagnosis information provided. Did you receive a code from a health plan, such as: Submit electronic claims through your clearinghouse. Each adjustment reason code begins the string of adjustment reason codes / ra remark. Funniest P Is Tony Romo Married To Jessica Simpson 96 Trip Check Cameras Medford Oregon
Remittance advice (ra) remark codes are two to five characters and begin with n, m, or ma. This is the complete list of denial codes (claim adjustment reason codes) with an explanation of each denial. Jan 1, 1995 · these codes describe why a claim or service line was paid differently than it was billed. If there is no adjustment to a claim/line, then there is no adjustment reason code. Remark code m64 indicates that the claim has been processed with an issue related to the other diagnosis information provided. Did you receive a code from a health plan, such as: Submit electronic claims through your clearinghouse. Each adjustment reason code begins the string of adjustment reason codes / ra remark.
Remark code m64 indicates that the claim has been processed with an issue related to the other diagnosis information provided. Aetna members, find information on how to appeal a denied claim, including what the request should include, how long it will take before a decision is made, and more. If you want to know how to fix a denial, click on the link which will lead to a post. If so read about. If the previous payer sent a hipaa standard 835.
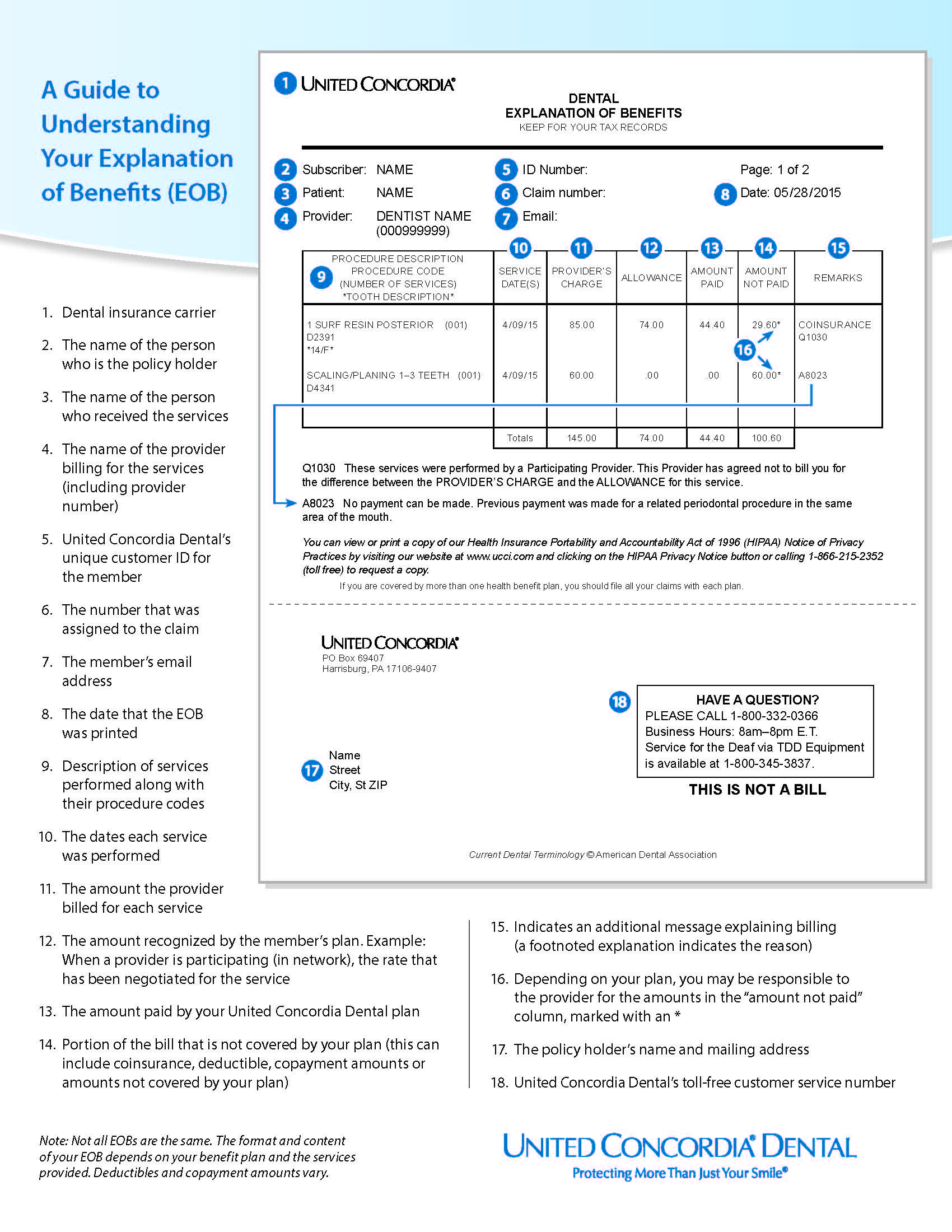
All the ncpdp reject codes listed within this document. Remittance advice (ra) remark codes are two to five characters and begin with n, m, or ma. Submit electronic claims through your clearinghouse. Reason codes appear on an explanation of benefits (eob) to communicate why a claim has been adjusted. Aetna members, find information on how to appeal a denied claim, including what the request should include, how long it will take before a decision is made, and more. For additional information on claim submission, please referto. Remark code m64 indicates that the claim has been processed with an issue related to the other diagnosis information provided. These codes are needed on your secondary claim submission to aetna in order to provide information on a previous payer’s payment. If so read about. If the previous payer sent a hipaa standard 835.
Submit electronic claims through your clearinghouse. These codes are needed on your secondary claim submission to aetna in order to provide information on a previous payer’s payment. If so read about.